I found this article interesting from the standpoint that we have never done this before and it is the beginning that could lead to curing cancer and more.
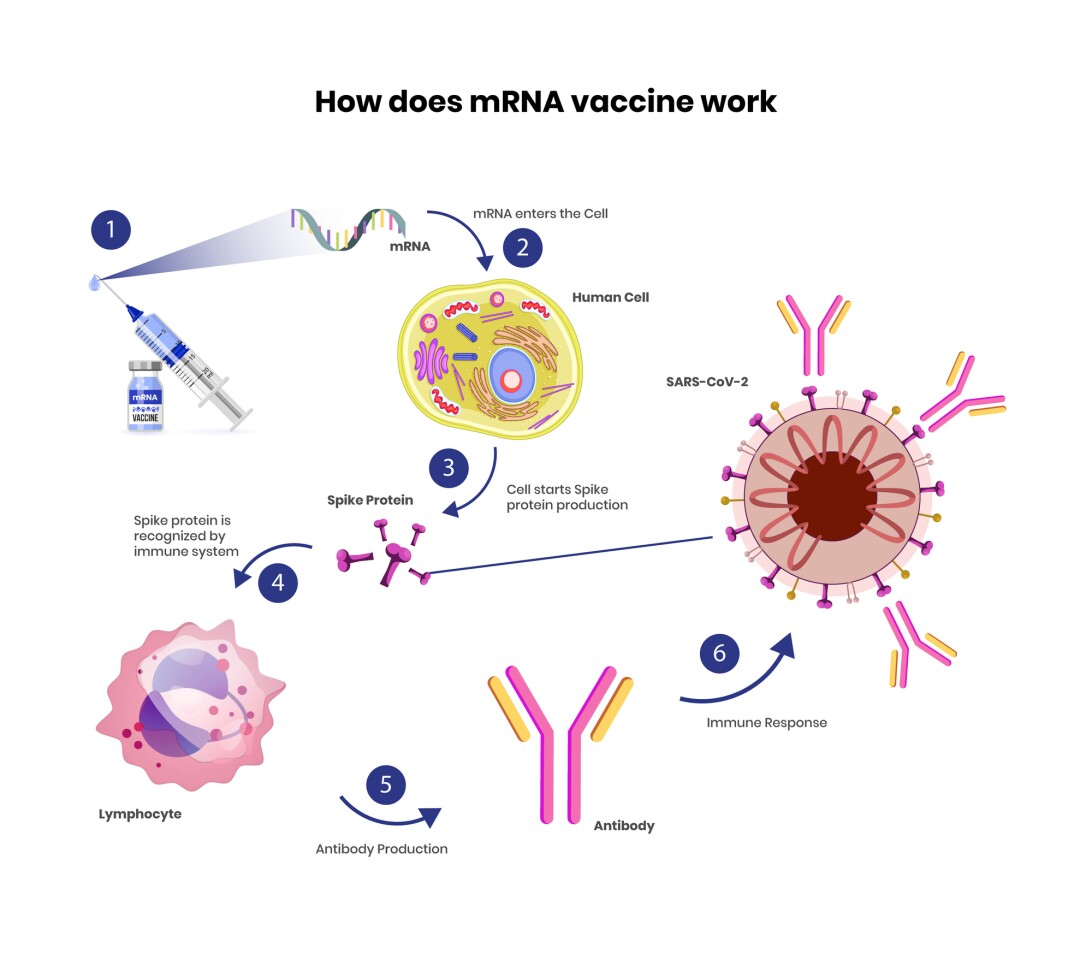
Over the past few months several hundred million people around the world have safely received a wildly effective COVID-19 vaccine based on mRNA technology that was still relatively experimental just one year ago. But what exactly is an mRNA vaccine, where did the technology come from, and what other diseases could it be useful for?
Despite the seemingly sudden appearance of this cutting-edge mRNA technology it is, like many scientific innovations, actually the product of decades of piecemeal research. mRNA was first discovered around 60 years ago after scientists worked for years trying to understand how DNA co-ordinated protein production in cells.
For decades scientists suggested it was hypothetically possible to hijack this mechanism and deliver artificially designed mRNA to a cell, instructing it to generate whatever protein one wanted. But the idea was science fiction until several discoveries in the 1980s finally made it possible.
Of course, once scientists started experimenting with their own forms of mRNA they discovered a new roadblock. Immune systems are clever. They are well geared to detect foreign bodies trying to infiltrate the body, and early animal studies revealed synthetic mRNA triggered profoundly fatal inflammatory responses.
Across the 1990s mRNA technology sat on the fringes of science, with many researchers suspecting the immune problem was insurmountable, but in 2005 biochemist Katalin Karikó published an extraordinary breakthrough. After toiling for well over a decade, she and colleague Drew Weissman demonstrated a small molecular tweak to synthetic mRNA that could allow it to evade immune defenses, slip inside a cell and send its message to the protein factories.
This ground-breaking discovery ultimately led to the founding of a pair of now well-known biotech companies, Moderna and BioNTech. But the ongoing research continued to strike hurdles. Karikó’s innovative discovery seemed to avoid triggering immune responses in animals when delivering low doses of synthetic mRNA, but any kind of ongoing administration with larger doses still triggered dangerous inflammatory reactions.
So, many researchers pivoted to investigating synthetic mRNA as a novel vaccine technology, since vaccines generally require just one or two small doses. Vaccines were never the primary focus for many mRNA researchers, however, they did seem to be the most feasible and realistic clinical application.
Alongside all of these innovations, nanoparticle research was accelerating in the 2010s, and this introduced a perfect solution to another problem facing mRNA researchers. mRNA molecules are fundamentally built to be temporary. They get inside a cell, deliver the necessary message, and then quickly degrade.
So, synthetic mRNA needs to be encapsulated inside something else to remain protected while it moves from factory to fridge to human cell. The solution came with the development of novel lipid nanoparticles. These nanoparticles protect the mRNA from degradation while also effectively slipping through a cell’s wall, helping deliver the mRNA right to the door of the cell’s protein factory.
All of these innovations and discoveries helped pave the way for mRNA technology to be uniquely ready for what was going to strike the world last year.
The pandemic acceleration
Developing a new clinical therapy can be a frustratingly slow process. The path from initial discovery to market approval for a new medicine can take at least a decade, with the three-phases of human clinical trials alone taking up tens of millions of dollars and more than six years to complete.
By 2019 mRNA vaccine research was quietly chugging along, with a number of targets proving promising in early-stage clinical trials. However, no mRNA-based therapy had yet been approved for market use and few people around the world had ever been administered this experimental treatment.
Harry Al-Wassiti, a bioengineer from Monash University, has been working with mRNA technology for several years, and he describes the pace and scale of mRNA manufacturing and distribution across 2020 as remarkable.
“Many of the innovations currently used by COVID-19 vaccines were developed throughout the past 12 years – but when COVID-19 hit, the best of those innovations and knowledge were put together,” Al-Wassiti tells New Atlas. “This is what makes this field amazing: it requires different innovations and expertise to solve the puzzle.”
On January 10 last year Chinese researchers published the genetic sequence of a novel coronavirus that had recently appeared in Wuhan. This was all mRNA scientists needed to begin work on a potential vaccine. By mid-February Moderna was first out of the gate with an experimental vaccine being shipped out for early-stage human clinical trials.
A little over a year later hundreds of millions of people have been given this vaccine. And while other COVID-19 vaccines have been developed over the past year, none have rivaled both the efficacy and safety profile demonstrated by mRNA vaccines.
More than just a COVID-19 vaccine
Thomas Preiss, a professor of RNA biology from the Australian National University, has been working in the field for more than 25 years. It was perhaps little surprise to Preiss that mRNA technology was this close to reality, after so many years of prior research laying the groundwork for the 2020 acceleration. But he does view the last year as a real turning point for the technology.
“The pandemic has greatly accelerated the transfer of mRNA therapies into a clinical reality,” says Preiss in an email to New Atlas. “Given how strongly the mRNA vaccines are performing, I expect this to be a real watershed moment for the technology and we will see other vaccines but also therapies for other diseases becoming available in the near future.”
It is these other applications Preiss alludes to that really reveal the revolutionary potential of mRNA technology. More than introducing just a new kind of viral vaccine, this technology could hypothetically be applied to an incredibly broad assortment of applications.
Cancer is one application many mRNA researchers have been investigating for years, and the current acceleration in the field will certainly help speed up ongoing studies. Al-Wassiti says these mRNA cancer treatments can be called “therapeutic vaccines.”
“Those act in a similar fashion to the viral vaccine, to train the immune system to recognize ‘existing’ cancer by vaccinating against molecules present predominantly in cancer but not healthy cells,” explains Al-Wassiti. “Other approaches may use mRNA to make ‘antibodies’ that target cancer or stimulate the immune system to fight cancer. The current understanding is that those ‘vaccines’ will complement existing therapeutics to improve the chance of survival.”
Viral vaccines and new cancer therapeutics are just the tip of the iceberg when it comes to the potential for mRNA therapies. Al-Wassiti says these targets are “low-hanging fruit,” with pre-existing research easily built upon. Auto-immune diseases, metabolic diseases, and respiratory inflammatory diseases all present novel opportunities for mRNA interventions. Even gene editing therapies such as CRISPR could be improved using mRNA technology.
“… the CRISPR guide is already a (short) RNA,” Preiss explains, “[so] the requisite Cas protein could be co-delivered as mRNA and the cells then translate it to generate the CRISPR-Cas ‘gene scissors.’”
The challenges ahead
Despite the extraordinary success of the COVID-19 mRNA vaccines over recent months, there are still big problems that need solving before this technology can be broadly applied to other diseases.
“As always with genetic medicines, the key hurdles are to solve effective and tissue-targeted delivery,” notes Preiss. “This is a comparatively minor issue with vaccines, but increasingly more important when the goal is to engender sustained therapeutic protein expression to treat non-infectious disease.”
Researchers now know mRNA technology works in the context of viral vaccines. But how to deliver these manufacturing blueprints to specific cells or organs is a whole new challenge.
“There is a common saying in gene and mRNA therapy: ‘delivery, delivery, delivery,’ this is because mRNA need not only [provide] protection but also delivery to specific organs,” says Al-Wassiti. “Delivery technologies will be a major development that will improve the technology further.”
It’s difficult to predict exactly how influential mRNA technology will be on medical science over the coming decade. What is undeniably clear though is how quickly this technology has moved from the experimental fringes into the mainstream.
Along with this greater attention comes increased funding for research and manufacturing. In the past it hasn’t been cheap to manufacture mRNA products, but that is rapidly changing. As the technology rapidly scales up and new researchers are attracted to the field it is fair to suggest the mRNA boom has begun.
Eighteen months ago the amount of humans administered with synthetic mRNA therapies numbered in the thousands. Now, that number is in the hundreds of millions. The technology has presented humanity with a pathway out of the worst pandemic in a century, and potentially this is only just the beginning of the mRNA therapy story.
Stay Safe!!